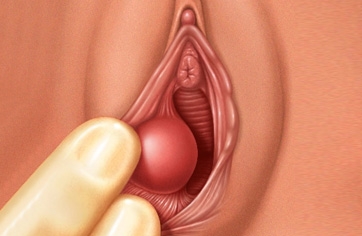
The Bartholin glands are pea-shaped structures located on either side of the vaginal opening. These glands secrete a fluid that helps with vaginal lubrication. Sometimes, the duct of these glands becomes blocked, causing the fluid to accumulate within the gland. This results in relatively painless swelling known as a Bartholin cyst. If the fluid inside the cyst becomes infected, it turns into a collection of pus surrounded by inflamed tissue, a condition called a Bartholin abscess.
A Bartholin cyst or abscess is a common condition. The treatment of a Bartholin cyst depends on its size, how painful it is, and whether it is infected. Sometimes, outpatient needle drainage is sufficient. In other cases, surgical drainage of the Bartholin cyst is required. If an infection occurs, antibiotics along with drainage can help treat the infected Bartholin cyst.
If the Bartholin cyst is small and not infected, it may go unnoticed. If the cyst grows, it may be felt as a lump or swelling near the vaginal opening. The cyst is usually painless, but it may be sensitive to touch.
An infection of the Bartholin cyst may develop within a few days. If the cyst becomes infected, the following symptoms may occur:
A Bartholin cyst or abscess typically occurs on one side of the vaginal opening.
Doctor's Visit
If you have a painful lump near the vaginal opening that does not improve within two or three days, contact your doctor. The pain associated with the cyst can be mild or severe.
If a new lump develops near the vaginal opening and you are over 40 years old, it is important to consult your doctor for an examination. Although rare, such lumps may be a sign of a more serious issue, such as cancer.
The cause of a Bartholin cyst is the accumulation of fluid produced inside the gland. Problems in the gland's duct, infection, or injury can lead to blockage and fluid accumulation. If a Bartholin cyst becomes infected, it can form an abscess. Bacteria such as Escherichia coli (E. coli),gonorrhea, and chlamydia, which cause sexually transmitted infections, can lead to infection and abscess formation in the gland.
Complications of Bartholin cysts include:
There is generally no way to prevent a Bartholin cyst.
However, practicing safer sex, especially using condoms, and maintaining good hygiene habits can help prevent infection and abscess formation in the cyst.
To diagnose a Bartholin cyst, the following examinations and tests may be performed:
Especially if the cyst is small and shows no symptoms, it may not require treatment. Treatment depends on the size of the cyst, the level of discomfort, and whether it is infected. Infected cysts should be treated as soon as possible.
Treatment options include:
The Bartholin glands are small, pea-shaped glands on each side of the vaginal opening that secrete fluid to lubricate the vagina. If the ducts become blocked, the fluid can accumulate, leading to cyst formation. An infected Bartholin cyst can lead to an abscess. When an abscess forms, there is intense pain, redness, and swelling on one side of the vagina. Abscesses can range from very small to 2-3 centimeters in size.
Approximately one in every 50 women has a history of a Bartholin cyst or abscess. Women of childbearing age, particularly those in their 20s, are most at risk. Bartholin abscesses occur when one of the glands becomes infected by Escherichia coli (E. coli) or sexually transmitted infections (such as Chlamydia and Gonorrhea).
More than 60% of women with Bartholin abscesses have bacterial infections. The most commonly seen bacterium is E. coli, responsible for 40-45% of infections. Bacteria are also significantly more common in cases of recurrent infections. In nearly 8% of cases, multiple types of bacteria are involved.
The most common bacteria associated with abscess formation are:
Other bacteria involved in abscess formation include:
Abscesses tend to be very painful. Typically, individuals with a Bartholin abscess experience pain only on one side of the vagina (on the infected gland side).
Other symptoms include:
If the abscess becomes large enough, it may rupture and drain pus. The person may notice vaginal discharge or a reduction in pain.
Surgical drainage is typically performed in a doctor's office or hospital. The doctor may use local anesthesia to numb the area or general anesthesia to put the person to sleep. During the procedure, the doctor makes a small opening in the abscess, allowing the fluid to drain. A catheter (a small plastic tube) is placed in the opening, and it may remain in place for up to 6 weeks.
The catheter helps keep the incision open, allowing all the fluid to drain. After the required time, the doctor may remove the catheter.
Marsupialization, a procedure, can help prevent recurrent Bartholin abscesses. First, the doctor makes a small incision in the abscess and drains it. Then, stitches are placed on both sides of the incision to create a permanent opening, usually no longer than 6-7 mm.
Sometimes, a catheter may be placed in the cavity for a few days to speed up the drainage process. Marsupialization is usually successful. Approximately 5-15% of Bartholin cysts may recur after the procedure.
If abscesses recur after marsupialization, Bartholin gland removal may be required. However, this procedure is considered a last resort and is rarely necessary. If needed, the procedure is performed under general anesthesia in a hospital. As with all surgeries, there are risks of bleeding, infection, and other complications.
Antibiotics can clear any infection present in the glands. Doctors often prescribe antibiotics before or after Bartholin gland surgery. Antibiotics may not always be necessary if the abscess has drained completely and does not recur.
Sitz baths can help relieve pain and discomfort. They can also assist in opening and draining very small abscesses. To perform a sitz bath, fill a bathtub with warm water and soak for about 15 minutes. This treatment is typically repeated at least 3-4 times a day until symptoms subside.
It is not always possible to prevent the development of a Bartholin abscess. However, certain precautions can be taken to reduce the risk of infection: